Sponsored: I will never forget hearing about my dad, driving down a winding mountain road while out of town for work, and he had to find a place to pull over and call 911 because he was having a heart attack. Thankfully, he was able to find a place to pull over and get the help he needed. Had he not been able to pull over, he could have hurt others on the road.
Table of Contents
Life Changes
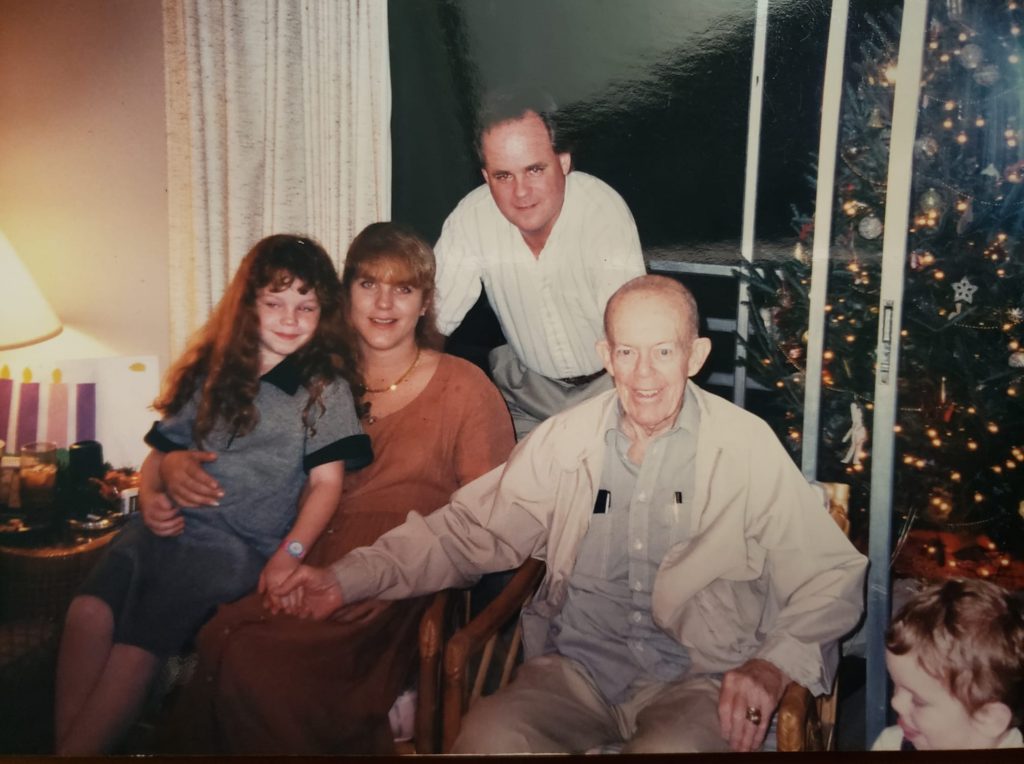
Life changes once you have a heart attack, and your journey may no longer look like you thought. I have watched my father and grandfather struggle with high bad cholesterol (LDL) even though they watched what they ate and lived active lifestyles.
My grandfather and father had no problem eating healthier thinking this would help impact their high bad cholesterol levels. But, unfortunately, some people, like my dad and grandfather, need more. The good news is people who have recently had a heart attack can manage high bad cholesterol through diet, exercise and medication management (if needed) and still enjoy their lives.
High Bad Cholesterol
High bad cholesterol is a problem for many folks, even though they eat healthily and exercise. Through no fault of their own, their high cholesterol numbers can persist due to their genetics.
That is the challenging part; you can do everything right and still have high bad cholesterol. I am sure there were many times my dad just wanted to have a steak or grill out with friends. And this is ok! You don’t have to give up what makes you feel human while maintaining a healthy lifestyle.
Here are some important things you need to know about cholesterol:
- Low-density lipoprotein (LDL) cholesterol is often called bad cholesterol. The reason LDL is called bad cholesterol is that it can build up in the walls of your arteries and form plaque, putting you at risk of a serious cardiovascular event, like a heart attack.
- High-density lipoprotein (HDL) is considered “good” because this type carries bad cholesterol away from the arteries.
A Treatment Option
It is essential to communicate with your doctor, eat right and have the right cholesterol-lowering medicines, if your doctor prescribes them.
Recently, I have learned about Repatha® (evolocumab). Repatha®, is a breakthrough medication that can help dramatically lower bad cholesterol and reduce the risk of a heart attack in adults with heart disease.
You can learn more by speaking with your healthcare provider about treatment options. For more information about Repatha®, visit Repatha.com
I am not a Repatha® patient and I do not have high cholesterol. I was compensated for this post.
IMPORTANT SAFETY INFORMATION
Do not use Repatha® if you are allergic to evolocumab or to any of the ingredients in Repatha®.
Before you start using Repatha®, tell your healthcare provider about all your medical conditions, including if you are allergic to rubber or latex, are pregnant or plan to become pregnant, or are breastfeeding or plan to breastfeed. The needle covers on the single-dose prefilled syringes and the inside of the needle caps on the single-dose prefilled SureClick® autoinjectors contain dry natural rubber. The single-dose Pushtronex® system (on-body infusor with prefilled cartridge) is not made with natural rubber latex.
Tell your healthcare provider or pharmacist about any prescription and over-the-counter medicines, vitamins, or herbal supplements you take.
What are the possible side effects of Repatha®?
Repatha® can cause serious side effects including serious allergic reactions. Stop taking Repatha® and call your healthcare provider or seek emergency help right away if you have any of these symptoms: trouble breathing or swallowing, raised bumps (hives), rash or itching, swelling of the face, lips, tongue, throat or arms.
The most common side effects of Repatha® include: runny nose, sore throat, symptoms of the common cold, flu or flu-like symptoms, back pain, high blood sugar levels (diabetes) and redness, pain, or bruising at the injection site.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Repatha®. Ask your healthcare provider or pharmacist for more information. Call your healthcare provider for medical advice about side effects.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.
Approved Use
What is Repatha®?
Repatha® is an injectable prescription medicine used:
- in adults with cardiovascular disease to reduce the risk of heart attack, stroke, and certain types of heart surgery.
- along with diet alone or together with other cholesterol-lowering medicines in adults with high blood cholesterol levels called primary hyperlipidemia (including a type of high cholesterol called heterozygous familial hypercholesterolemia [HeFH]) to reduce low-density lipoprotein (LDL) or bad cholesterol.
Please see full Prescribing Information https://bit.ly/37KUHBe and Patient Product Information https://bit.ly/3rkiXAQ.
© 2021 Amgen Inc. All rights reserved.
These statements have not been evaluated by the Food and Drug Administration. Any product(s) on this website is not intended to diagnose, treat, cure, or prevent any disease.
Always consult a licensed health care professional before starting any supplement or nutraceutical. Especially if you are pregnant or have any pre-existing medical conditions. Individual results may vary. These are from my own experience and the experience of others and only our opinions.




